Contributor:
Teddie Potter PhD, RN, FAAN
School of Nursing University of Minnesota
tmpotter@umn.edu
Throughout the history of professional nursing, nurses have designed new care delivery models and transformative interventions in response to unmet needs and population health and public health challenges. These changes required disruptive thinking and bold courage in the face of broken systems, ineffective policies, and powerful naysayers. Climate change may be a modern example of a major public health crisis yet the challenges to mounting an effective response are similar. This is the story of Nurses Drawdown, a global, nurse-led movement to improve the health of humans and the planet.
Honoring the Ancestors of this Movement
Around the globe, the earliest experts in planetary health were, and continue to be, indigenous people. Their values and patterns of decision-making acknowledge the deep interconnection of human health and the health of the biosphere.
Many early nursing leaders shared a similar awareness that we ignore the environment at our peril. The ideas of Florence Nightingale, Lillian Wald, and Mamie Odessa Hale offer inspiration to transformative leaders today. Florence Nightingale is considered the founder of modern professional nursing; her astute observations and applied statistics established nursing as a science-based profession. Nightingale was an expert systems thinker who connected the health of humans to the quality of the environment. Like Florence, nurses today must recognize that nursing care is delivered in the context of nature.

Lillian Wald, the founder of public health and school nursing, faced the daunting task of addressing the health needs of resource-poor immigrants in New York City (Wald, 1915). She went to the people and lived among them. Her willingness to participate in health initiatives alongside those she served offers a lesson for transformative leaders today. Nurses can inspire people to take action on climate change by first making changes in their own lives.

Source
Mamie Odessa Hale was another historical change agent. Hale was an African American Nurse Midwife practicing in an era of deep racial segregation. She taught community midwives simple practices based on the best science of the time thereby improving birth outcomes for African Americans (Hale, 1948). The story of Mamie Odessa Hale encourages today’s nurses to realize that simple science-based interventions, taught with respect and empathy, can transform the health of individuals and whole communities.
These early nursing leaders laid the foundation for today’s global movement to address climate change. They are a part of the Nurses Drawdown story.
The Seeds of a Movement
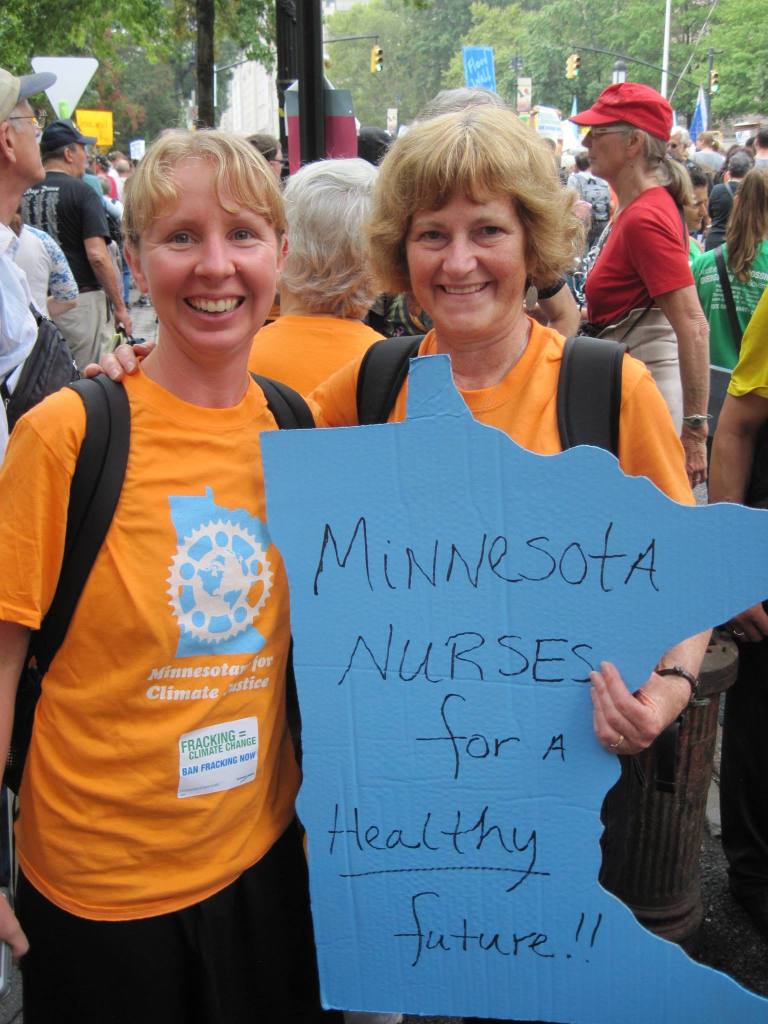
In September 2014, I took a long bus trip across the nation to attend the People’s Climate March in New York City. Over half a million people from all demographics and all walks of life came together to send a strong message that the United States must take climate change seriously and meaningfully contribute to global negotiations.
Like my fellow travelers from Minnesota, I wore a bright orange t-shirt. The only indication that I was a nurse was the sign I created that said, “Minnesota Nurses for a Healthy Future.” As the march moved through the streets of Manhattan, I was shocked how frequently observers standing along the route commented to one another, “The nurses are here!” Some even asked to take their picture with me so they could send it out on social media with the message that nurses had shown up to address climate change. I remember thinking, “What is this?” The people were not shouting, “The engineers are here!” or “The teachers are here!” There is something about nurses taking on climate change that inspired hope.
Fast forward to 2018 when I adopted the book Drawdown: The Most Comprehensive Plan Ever Proposed to Reverse Global Warning (Hawken, 2017) for “The Global Climate Challenge: Creating an Empowered Movement for Change,” a course that I teach at the University of Minnesota. Climate change is an urgent public health crisis; therefore, I teach that our solutions must be effective and have significant impact. Project Drawdown (2020)provides the solutions; could nurses provide the inspiration to scale them?
I contacted Project Drawdown and presented the argument that as the largest global health profession and the most trusted profession, nurses may be able to effectively and broadly scale Project Drawdown’s science-based solutions to climate change. Nursing’s long history of innovative leadership to improve the health of individuals, families, and communities can be relied on to improve the health of humans and the health of the planet. So, a partnership was formed between Project Drawdown and the Alliance of Nurses for Healthy Environments (ANHE).
ANHE (2019), the leading professional organization for nurses working to promote a healthier environment, coordinates the Nursing Collaborative on Climate Change and Health, a broad network of professional organizations committed to planetary health. Katie Huffling and Cara Cook from ANHE and I assembled a leadership team to plan and initiate Nurses Drawdown. It was very important that we include nurses across the globe, nurses from a wide variety of practice settings, and different demographics including nursing students.
Nurses Drawdown
The vision for Nurses Drawdown is “to improve the health of individuals, communities, and the planet through commitment to and action on the Nurses Drawdown solutions.” The mission is, “Nurses, the most numerous and most trusted health profession in the world, have the power to significantly impact climate change. By embracing and teaching the evidence-based solutions of Nurse’s Drawdown, nurses around the world will help to decrease greenhouse gas emissions and create a healthier future for humans and the rest of the planet.”
To this end, the Nurses Drawdown leadership team elected to scale Project Drawdown solutions that have the co-benefits of improving human health and the health of the planet. We selected five themes, reflecting an alignment between core nursing expertise and effective evidence-based solutions. These include:
- FOOD: Committing to eat a more plant-based diet, using clean burning cookstoves, and reducing food waste
- MOBILITY: Promoting walkable cities, including improving bike infrastructure and using mass transit
- GENDER EQUITY: Educating girls and improving access to family planning
- ENERGY: Increasing the efficiency of buildings and transitioning to clean energy sources
- NATURE-BASED SOLUTIONS: Planting trees and protecting forests
An Invitation to Join the Movement
Throughout history, professional nurses have been at the forefront of change. Whether it was alleviating mass suffering related to conditions of war, addressing severe economic disparities that impact health, or responding to new and emerging infectious diseases, nurses’ orientation toward systems thinking and prevention have made them the ideal leaders for innovating and mobilizing effective solutions.
We invite you to continue this tradition by joining Nurses Drawdown at nursesdrawdown.org. Under the Take Action tab, you will find practical solutions to apply in both your personal and professional life. You will also be inspired by the stories of nurses around the globe who are taking action to promote a healthier future for generations to come.
Many will remember 2020 as the year of the pandemic. Let them also remember 2020 as both the Year of the Nurse and Midwife (World Health Organization, n.d.), and the year that nurses around the globe activated to address climate change. The nurses are here!
References
Alliance of Nurses for Healthy Environments [ANHE]. (2019). Alliance of Nurses for Healthy Environments. https://envirn.org/nursing-collaborative/
Hale, M. O. (1948). Arkansas midwives have all-day graduation exercises. The Child, 13(4): 53–54.
Hawken, P. (2017). Drawdown: The most comprehensive plan ever proposed to reverse global warning. New York, NY: Penguin.
Project Drawdown. (2020). Drawdown 2020. https://www.drawdown.org/
Wald, L. (1915). The house on Henry Street. New York: Henry Holt.
World Health Organization. (n.d.). Year of the nurse and midwife 2020.https://www.who.int/campaigns/year-of-the-nurse-and-the-midwife-2020
About Teddie M. Potter, PhD, RN, FAAN

- Clinical Professor, School of Nursing- University of Minnesota
- Specialty coordinator of the Doctor of Nursing Practice in Health Innovation and Leadership
- Director of Planetary Health
Dr. Potter is deeply committed to climate change education including co-founding Health Professionals for a Healthy Climate, membership in the Alliance of Nurses for Healthy Environments, and membership on the American Academy of Nursing Environment and Public Health Expert Panel. She is a member of the Coordinating Committee of Columbia University’s Global Consortium on Climate and Health Education and a Fellow in the Institute on the Environment at the University of Minnesota. She chairs Clinicians for Planetary Health (C4PH) and is a member of the Steering Committee of the Planetary Health Alliance at Harvard.
At the University of Minnesota, Dr. Potter designed and co-teaches an interdisciplinary course titled “The Global Climate Challenge: Creating an Empowered Movement for Change”. In addition, she co-leads a Health Sciences initiative titled, “Climate Change and Health: An Interprofessional Response”. In 2019, Dr. Potter was appointed the first Director of Planetary Health for the School of Nursing.

 Nurses also took action by protesting outside of the Whitehouse on April 21 and reading aloud the names of nurses who died from contracting COVID19 in the workplace:
Nurses also took action by protesting outside of the Whitehouse on April 21 and reading aloud the names of nurses who died from contracting COVID19 in the workplace: