Like many of you reading this, I have a range of emotions and feelings as the pandemic of COVID19 grows in the USA: anxiety, fear, and anger. Today (and for the last several days), I am angry about the lack of Personal Protective Equipment (PPE) available for nurses who are being called to care for those who are most ill and the most contagious. The following is my attempt to express my personal concerns and align them with nursing’s guiding ethical principles.
There may be flaws in my thinking and I am open to respectful dialog about these issues. I understand that emotions are running high and that we may not agree, but we can and should have civil discussions and dialogs.
Lack of Personal Protective Equipment. On February 7, 2020, the World Health Organization warned of a shortage of Personal Protective Equipment in China and beyond. As that was 6 weeks ago, there has been time to ramp up the production of PPE. Meanwhile, state’s governors from Maine to Wisconsin to Florida and Washingon are asking to access the federal stockpiles for access to PPE:
Nurses Quitting: A few days ago, one of my Facebook friends quit her job because she was no longer being provided the proper PPE, She was not directly caring for COVID19 patients, but she needs proper PPE to keep herself and her patients safe during the provision of care, and her quitting her job got me thinking, considering ethical issues, advocacy, the role of the nurse, and so on. I respect her decision, and I hope this post makes it clear that during these frightening and murky times, the decisions we make as nurses are going to be hard ones.

I want to say, from an ethical perspective, it is perfectly acceptable for nurses to quit their jobs and/or refuse to work without proper PPE. Refer to my previous post of the ANA calling for the CDC to provide evidence when they make guidelines, and consider the recent use of bandanas and reuse of face masks protocol from the CDC: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html. This flies in the face of everything we know about the transmission of viruses.
Ethical Principles: The overarching ethical principles at play here that help to guide nurses’ decision making are beneficence (doing the good thing, moral obligation to do the right thing, what is best for the patient) and nonmaleficence (do no harm to patients). When we work without proper PPE, there is a very real risk that not only might we harm ourselves, we potentially spread pathogens to patients. When we don’t have proper PPE, our stress, fear, and anxiety can be magnified and potentially may harm patients.
Additionally, The code of ethics for nurses (https://www.nursingworld.org/coe-view-only) requires a lot of us. To begin with, we must be deeply familiar with The code and how it guides our decision-making processes. The following are some excerpts from The code that guide our decision making at this time:
The code: 3.5 Protection of Patient Health and Safety by Acting on Questionable Practice
This concept is all about the reporting of inappropriate and questionable practices. We may become stymied when even our boards of nurses are aware of dangerous and non-evidence-based practices, but they may see no way around them. We can report the issues, but when the governing bodies we report to are not holding up our own ethical standards, the field is put at greater risk for collapse (from infection spreading and/ or providers quitting).
Even as standards are relaxed, entities such as the Oregon Board of Nursing should be taking more responsible action and not placing nurses and patients at risk. The following is a statement by the Oregon Board of Nursing that states that nurses cannot refuse assignments because of sub-par PPE that does not align with CDC or WHO regulations. In other words, in this case, the BON is either not considering the greater harm for both patients and nurses by not recognizing the greater ethical concerns and personal risks nurses are being asked to take, or they simply see no other solutions. The paragraphs about the social contract and evidence-based approaches contradict the highlighted area regarding changes in PPE approaches and the right to refuse assignments.
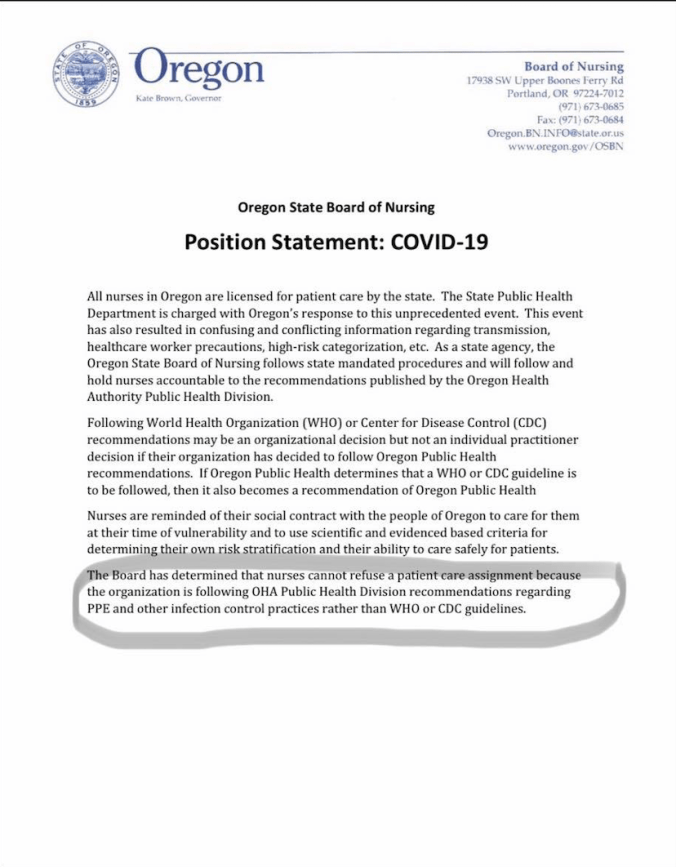
Regardless of what our boards of nursing state, Provision 4 makes it clear that we are ultimately responsible for our own practice: “The nurse has authority, accountability, and responsibility for nursing practice; makes decisions, and takes action consistent with the obligation to promote health and to provide optimal care”. Specifically, Provision 4.1 states that “Nurses bear primary responsibility for the nursing care that their patients and clients receive” and “Nurses must always comply with and adhere to state nurse practice acts, regulations, standards of care, and ANA’s Code…”. This does lead to interesting paradoxical issues with the Oregon Board of Nursing, as one could view this as a regulation, but it contradicts further statements in The code, including:
Provision 4.3: “Nurses are always accountable for their judgment, decisions, and actions: however in some circumstances, responsibility may be borne by both the nurse and the institution. Nurses accept or reject specific role demands and assignments based on their education, knowledge, competence, and experience, as well as their assessment of the level of risk for patient safety. Nurses in administration, education, policy, and research also have obligations to the recipients of nursing care” and “Nurses must bring forward difficult issues related to patient care and/or institutional constraints upon ethical practice for discussion and review”.
Most importantly, The code calls for us to take good care of ourselves so that we can take care of others. We see this shown in Provision 5, particularly:
Provision 5.2 Promotion of Personal Health, Safety, and Well-Being
“…nurses have a duty to take the same care for their own health and safety. Nurses should model the same health maintenance and health promotion that they teach and research, obtain health care when needed, and avoid taking unnecessary risks to health or safety in the course of their professional and personal activities.” The sticking point here is arguing whether or not the risks of not wearing proper PPE, which include risks of death for oneself or other patients who have not yet been exposed, is necessary or not. From my perspective, I can see where working without proper PPE could be too large of a risk to oneself and the communities served.
And I get concerned when nurses seem to think it’s only about them be willing to take on the personal risk for themselves, forgetting about how they may also become the vector.
One last ethical issue, we have to do our own self-care during these challenging times. As nurses, we are required to take care of ourselves. Provision 5.2 continues: “Fatigue and compassion fatigue affect a nurse’s professional performance and personal life. To mitigate these effects, nurses should eat a healthy diet, exercise, get sufficient rest, maintain family and personal relationships, engage in adequate leisure and recreational activities, and attend to spiritual or religious needs…it is the responsibility of nurses leaders to foster this balance within organizations”
Now onto a round-up of current COVID19 issues for nurses as I am seeing on social media:
Masks: Some nurses are being told to store their 1 daily mask in a paper bag and remove/ doff between patients, and replace/don the old mask for new patients. Of course, the bag and the mask would all be potentially contaminated; the bag actually creates a source of contamination and risks for greater transmission. I also heard rumors on social media of nurses being told to share masks, and I am hoping this is simply just false information, as I couldn’t verify that claim. I did hear that eye shields were being shared. I have confirmed that nurses who are normally required to wear masks because they have not been vaccinated for the flu are now being told to not wear masks because there is a shortage of masks. I have also confirmed that having a doctor’s note regarding why one must wear a mask (verification that they are immunocompromised) may work in some settings to either ensure masks are available to the person or excuse them from work.

We are vulnerable: Nurses are humans and many of us are vulnerable, whether that means we have chronic health conditions and co-morbidities, or we are at risk because of age.
- The average of RN’s in the USA is 50, perhaps increasing risks related to the virus (https://alliedstaffingnetwork.com/americas-nurses-are-aging/ ),
- Indeed it has been documented that healthcare workers may fair worse when they contract COVID19, which in part may be related to stress or multiple exposures to the virus. The healthcare system was already strained before the pandemic started, and as nurses also become ill, the system will become even more strained (https://www.businessinsider.com/nurses-are-understaffed-and-frustrated-as-they-battle-coronavirus-2020-3 ).
- We are already feeling the “psychic” shock of this pandemic, and showing signs of potential PTSD ( https://www.washingtonpost.com/outlook/2020/03/18/doctors-nurses-are-already-feeling-psychic-shock-treating-coronavirus/?fbclid=IwAR3yUXxn6VrwckM1p3FX1pAeBMARQ8hlxCMaUm_kr81b2xZB6aHLr2UBV9k ). I am seeing growing division of nurses on social media pages regarding many of these topics.
- I heard rumors that as many as 1/2 of the positive COVID19 cases in the state of Pennslyvania were healthcare providers. I couldn’t verify this fully, though there are positive healthcare providers (https://6abc.com/6026148/), and on this date, at least 10 of the 44 cases recently identified in PA are healthcare providers (https://patch.com/pennsylvania/chestnuthill/20-44-coronavirus-cases-philadelphia-are-healthcare-workers?fbclid=IwAR1o0fR0kLQA4aat1-qr1LU0UyxrWz3Gy_nVecEB3_QXgXc9c0cMghZCnAs ).
- We, of course, know that healthcare providers are at greater risk, and likely more so with poor PPE (https://www.washingtonpost.com/health/covid-19-hits-doctors-nurses-emts-threatening-health-system/2020/03/17/f21147e8-67aa-11ea-b313-df458622c2cc_story.html ).
- We are worried about our families, and this may mean distancing ourselves from them (https://www.advisory.com/daily-briefing/2020/03/18/doctor-fears) or choosing to protect the frail in our family instead of working. I have heard of nurses and doctors renting airb-n-b rooms to be away from their families in order to protect them from contamination.
- We are being denied sick leave after exposure or told to use PTO or go without pay. Or we are being told to work post-exposure, or work with flu and cold-like symptoms if no fever is present.
- For nurses who are willing and able to work, many believe they should be getting hazard pay for the risks they are willing to take.
Nurses are also fighting amongst themselves about whether it is okay to quit the workplace now. We have to recognize that these are complex decisions; nurses are real people who have their own health issues. Getting angry about people not willing to take the risk is not productive in both the short and long term.
It’s okay to choose your life and your well-being over the “duty” or social contract to work. It’s okay to make those tough decisions, like quitting your job, and, for some folks, they may be willing to risk their license by refusing assignments where they can’t keep themselves or their patients safe, even if their board of nursing disagrees.
Many nurses will carry on, work hard, provide excellent care, and do their best.
It’s also okay to feel vulnerable and scared in these uncertain times and to question your decisions and the decisions of administrators, regulators, and leaders.
It’s okay to organize and advocate for our needs, whatever that looks like.
Always remember, you have ethics on your side.